 “Depression is not a mood, it’s a disease.” – Unknown.
“Depression is not a mood, it’s a disease.” – Unknown.
A lingering and pervasive sense of sadness, emptiness, and apathy. Listlessness. An inability to take pleasure in fun, social activities. The impression that life is happening to you and around you at a slow, oppressive pace yet also slipping through your fingers. The inability to sleep or sleeping too much. Brain fog. Frustration. Self-loathing. Despair.
This tapestry of feelings is what Europeans tended to label “melancholia.” Though the exact definitions may have been refined and further distilled into an expansive list of mood orders since Johann Wolfgang von Goethe delved into the psyche of Young Werner, his contemporaries were more than prescient in labeling this affliction, depression, the modern malaise.
 With more than 18% of the American adult population having been diagnosed with depression and 11% prescribed antidepressant medication in 2025 according to a recent study, it’s a major health issue that calls for awareness. As these stats are higher for women when the numbers are parsed for sex/gender, it’s more than adjacent to many of our lifestyle, wellness, and beauty concerns and regiments. It’s hard to achieve vibrant health and beauty when under a fog of despair.
With more than 18% of the American adult population having been diagnosed with depression and 11% prescribed antidepressant medication in 2025 according to a recent study, it’s a major health issue that calls for awareness. As these stats are higher for women when the numbers are parsed for sex/gender, it’s more than adjacent to many of our lifestyle, wellness, and beauty concerns and regiments. It’s hard to achieve vibrant health and beauty when under a fog of despair.
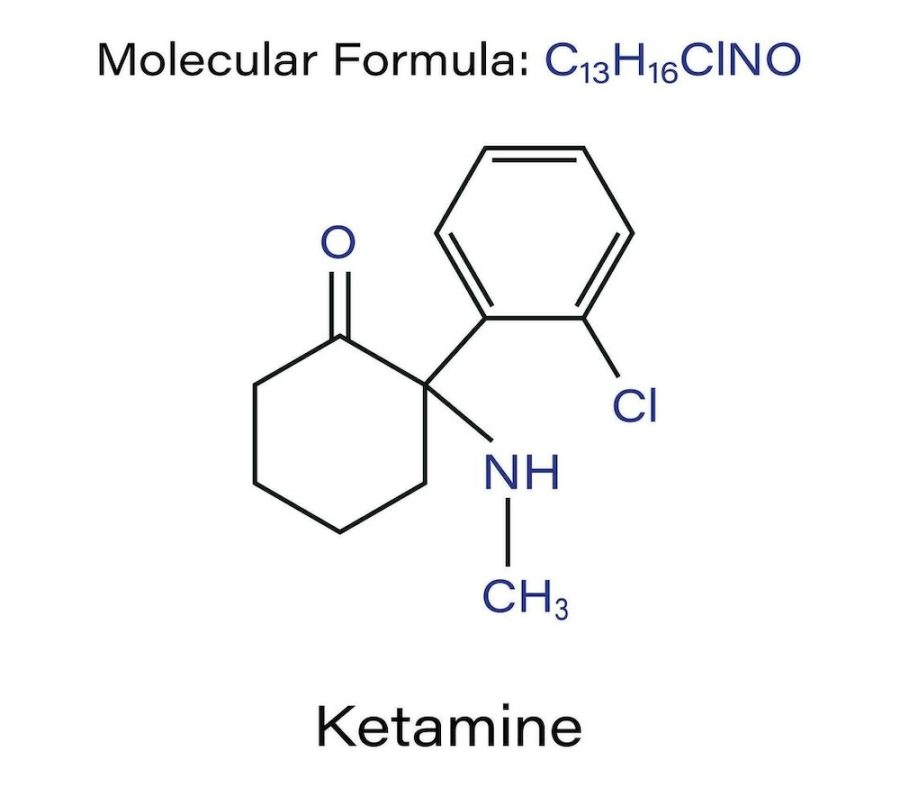
For World Mental Health Day, it was essential that I speak to Dr. Elaine Suderio, a health professional at the cusp of the buzziest innovation in depression treatment offered at the Hudson Valley Ketamine Lounge. While SSRIs have been the standard prescription for this mood disorder, lately its efficacy has been called into question by meta studies and the increasing number of patients who report hitting a wall with serotonin-based pills. Similar to the constant chatter about microdosing of psychedelics in the past decade, a substance typically associated with recreational use – ketamine – has been the focus of extensive research and practical applications.

1. The history of ketamine is fascinating. How did it morph from a horse tranquilizer to the preferred drug of Club Kids into a buzzy mental health innovation?
Ketamine was first developed in the 1960s and received FDA approval in 1970 for use as a human anesthetic. It became a vital tool during the Vietnam War, relied on to safely and effectively treat wounded soldiers in the field. Because of its high safety profile and reliable pain control, veterinary clinics soon also began using it as well; particularly for large animals like horses. This led to its misleading reputation as a “horse tranquilizer,” even though it was originally and still continues to be for human use.
By the 1980s – 1990s, ketamine found its way into the club scene. Recreational users sought its euphoric and dissociative effects. Despite the stigma that followed and almost de-railed the drug’s progress, researchers continued to explore its medical potential. In the early 2000s, studies revealed ketamine’s remarkable antidepressant properties, showing rapid and sustained relief for individuals with treatment-resistant depression.
By the 2010s, it became a legitimate clinical therapy across the U.S., helping patients manage mental health conditions and chronic pain. Now, in 2025, ketamine therapy is gaining widespread recognition as a breakthrough treatment in psychiatry and pain management. This is reshaping how we understand and heal the brain.
 2. Most antidepressants are SSRIs. Why are these proving less effective with depression than with anxiety disorders?
2. Most antidepressants are SSRIs. Why are these proving less effective with depression than with anxiety disorders?
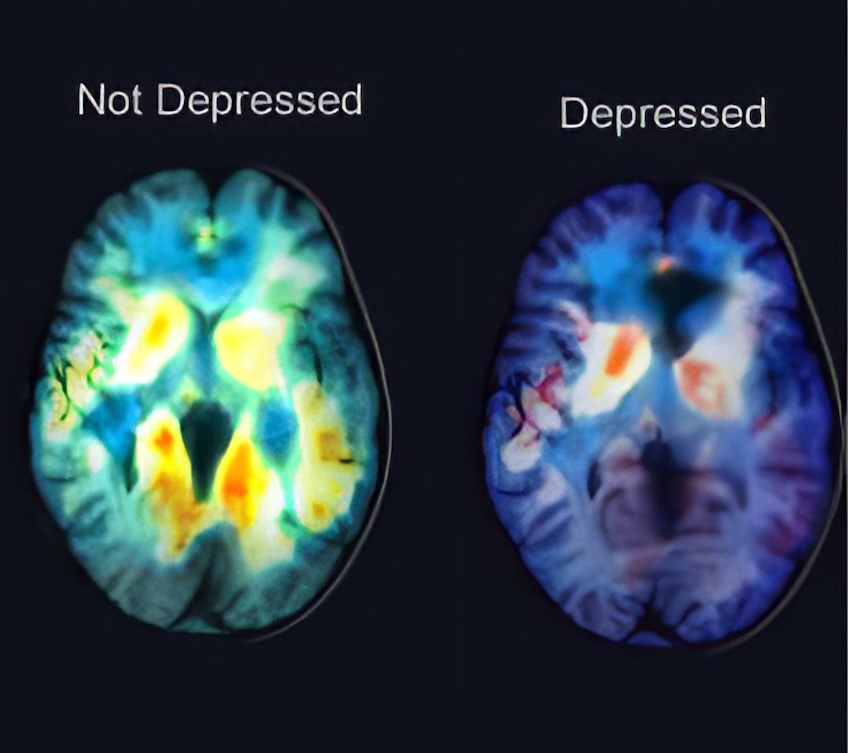
SSRIs can take several weeks to begin showing results and often come with uncomfortable side effects, especially at higher doses. Depression, however, is not just a serotonin problem. Low neuroplasticity can compromise your brain’s ability to adapt and repair, and disruptions in glutamate signaling can cause a loss of synaptic connections that regulate mood and motivation.
This is why traditional SSRIs may be less effective in treating depression when deeper neural issues are present. On the other hand, SSRIs can be highly effective for anxiety disorders, as increasing serotonin helps calm the body’s fight-or-flight response, reducing panic and fear while stabilizing an overactive nervous system.
 3. What Is the Difference between ketamine IV and KAP?
3. What Is the Difference between ketamine IV and KAP?
Ketamine IV is the process of intravenous infusion of the drug for a patient. KAP (ketamine assisted psychotherapy) builds on this as it would also use IV ketamine. KAP would just be adding a therapy session (psychotherapy) after treatment. This therapy session is typically performed post treatment and is found to drastically help patients process their thoughts, emotions and insights to make real lasting change. Having mental health providers that can help our patients work through their “roadblocks” is very important.
At Hudson Valley Ketamine Lounge, we are actively building a trusted network of therapists, social workers, and psychotherapists to better support our patients. Collaboration between medical and mental health providers is a required and integral part of our approach to care.
4. Can you explain ketamine therapy in laymen’s terms?
Ketamine therapy is a medical treatment that uses low doses of ketamine, traditionally an anesthetic, to alleviate symptoms of depression, PTSD, anxiety, chronic pain, and other mental health conditions. In our clinic, it is administered via intravenous (IV) infusion. Ketamine works in our bodies by rapidly increasing communication between brain cells. This is done because it increases glutamate activity and supports neural regeneration. This directly relates to sleep, relaxation, anxiety, and even muscle function. Patients report feeling lighter and have improved sleep after just the first treatment in their series. Ketamine is especially effective when it comes to chronic pain conditions as well. The nervous system becomes hypersensitive to pain when it has been chronic and continuous. Ketamine’s NMDA receptor-blocking properties help “reset” pain pathways and reduce pain levels at a neurological level. Comfort can improve within the first session in your series. Ketamine, in a clinically administered setting, has little to no addictive properties.
 5. Is ketamine infusion therapy a form of microdosing, similar to practices with cannabis and other psychedelics?
5. Is ketamine infusion therapy a form of microdosing, similar to practices with cannabis and other psychedelics?
No, ketamine infusion therapy is not considered microdosing. While the comparison sometimes comes up, it mainly stems from the fact that the doses used in mental health treatments are much lower than the anesthetic doses used in hospitals for surgical procedures. For a better idea, in hospitals usually 200mg is used in anesthesiology and for ketamine therapy around 50-100mg is used, determined on a case-case basis. During an infusion, patients receive a clinically calibrated dose of ketamine based on their weight and medical history. The goal is to achieve a therapeutic effect, promoting neuroplasticity and mood regulation; without causing full anesthesia. Depending on the individual and dosage, patients may remain alert and conversational or experience mild relaxation or dissociation during treatment. This is very different from the sub-perceptual “microdosing” practices seen with psychedelics or cannabis.
6. How exactly does ketamine work to lessen depression? Is the science of it fully understood?
How ketamine works is that it helps re-grow the pathways in your brain that control your glutamate system. This helps your brain function properly by increasing communication. Ketamine promotes neuroplasticity, this helps stimulate the growth of new synapses and repairs the damaged circuits that are caused by chronic stress and depression.
Typically with depression, the reason it occurs is there is a lack of communication from your neurotransmitters. Without being able to receive the necessary hormones plus add in stress, people tend to feel hopeless or emotionally numb. The more activity and movement between these synapses leads to proper dopamine and serotonin delivery; improving mood, sleep, motivation, and reducing brain fog.
7. Which other mental health conditions can ketamine treat?
Ketamine can treat depression, anxiety, PTSD, bi-polar disorder, and OCD. As the medical scene evolves, I am sure there will be more uses for this treatment.
 8. Who is the ideal patient for ketamine infusion therapy?
8. Who is the ideal patient for ketamine infusion therapy?
A person who has been struggling with treatment resistant mood disorders, having tried at least two different medications. A person who is struggling with Post Traumatic Stress Disorder (PTSD) will find this effective in helping resolve conflicts in therapy as well as improve sleeping and anxiety. For people suffering with chronic pain conditions, ketamine helps the brain restore.
9. What is the most common course of ketamine infusion therapy for depression?
For these cases, our protocol would be to perform a series of 4-6 infusion treatments over the course of 2-3 weeks based on the severity of symptoms. We find these series are most effective in patients and report drastic improvements post treatment.
10. What are the most common contraindications for ketamine infusion therapy? And side effects?
Ketamine infusion therapy is safe for most patients when properly screened and monitored. However, certain conditions may make treatment unsafe or inappropriate. There are also different contraindications based on mental health and medical history
A. Common Contraindications Medically:
- Uncontrolled hypertension or severe cardiovascular disease. Ketamine can temporarily raise blood pressure and heart rate.
- History of intracranial pressure or brain masses. Increased blood pressure during treatment could worsen these conditions.
- History of intraocular pressure. Ketamine could compromise vision and retinal nerve
- Pregnancy or breastfeeding. Not enough research to confirm safety for the mother or child.
- Active substance abuse. May increase risk of misuse or unpredictable reactions.
B. Relative Medical Contraindications:
- Seizure disorders. Could cause patient with history of seizure to induce a seizure, but also has anticonvulsant effects, the reason it is not a total contraindication
C. Mental Health Contraindications:
- Schizophrenia or active psychosis. Ketamine’s dissociative effects can intensify symptoms in these patients.
- Hyper-manic, bi-polar disease. Current manic ongoing episodes could worsen due to the effects of ketamine
**Before starting therapy, all patients undergo comprehensive medical and psychological screenings to ensure safety and optimal outcomes.
11. How painful is the treatment?
Most patients find the treatment very comfortable. The only momentary discomfort may come from placing the IV catheter, similar to having blood drawn. Our team of skilled and gentle medical professionals ensures the process is quick and as painless as possible. Once the infusion begins, patients typically relax and rest comfortably for the duration of the session.
 12. Is ketamine infusion therapy covered by most health insurance providers?
12. Is ketamine infusion therapy covered by most health insurance providers?
At this time, most insurance providers do not cover ketamine infusion therapy, though some may reimburse a portion of the cost depending on your plan. Currently, only the nasal spray form of ketamine has FDA approval for depression and is typically eligible for coverage. However, IV infusions are more effective because they provide 100% bio-availability, meaning the medication is fully absorbed into the bloodstream, allowing for more consistent and lasting therapeutic results.
13. How does Hudson Valley Ketamine Lounge approach ketamine infusion therapy?
Our approach to ketamine treatment is to focus on the patient’s clinical needs. We will have new patients fill out a thorough medical history, mental health screening assessments and ketamine intake form. Based on these tools, another one of our providers, Dr. Miller provides the initial consultation to speak with the patient. If approved for treatment, we typically offer a series of treatments based on the protocol needed for the client’s specific case: chronic pain conditions, mood disorders or PTSD. We require the patient to have a therapist as it is proven that connecting the mind to the body’s response is imperative for real lasting change. We always encourage patients that are already established with a therapist, psychologist, social worker, etc. to have us connect to offer the most effective treatment. We have started and will continue to grow a network of mental health providers to help ensure our patients are well taken care of. We continue to stay connected to our patients and will check in to follow up with their progress.
If suffering from depression and curious about this course of treatment, contact the Hudson Valley Ketamine Lounge to begin the intake process.
Be well!!

